Cpt code dating ultrasound
Randomized and quasi-randomized controlled trials of Doppler ultrasound for the investigation of umbilical and fetal vessels waveforms in unselected pregnancies compared with no Doppler ultrasound were selected for analysis. Studies where uterine vessels have been assessed together with fetal and umbilical vessels have been included. Two review authors independently assessed the studies for inclusion, assessed risk of bias and carried out data extraction. In addition to standard meta-analysis, the 2 primary outcomes and 5 of the secondary outcomes were assessed using GRADE software and methodology.
These researchers included 5 trials that recruited 14, women, with data analyzed for 14, women.
All trials had adequate allocation concealment, but none had adequate blinding of participants, staff or outcome assessors. Overall and apart from lack of blinding, the risk of bias for the included trials was considered to be low. Overall, routine fetal and umbilical Doppler ultrasound examination in low-risk or unselected populations did not result in increased antenatal, obstetric and neonatal interventions.
There were no group differences noted for the review's primary outcomes of perinatal death and neonatal morbidity.
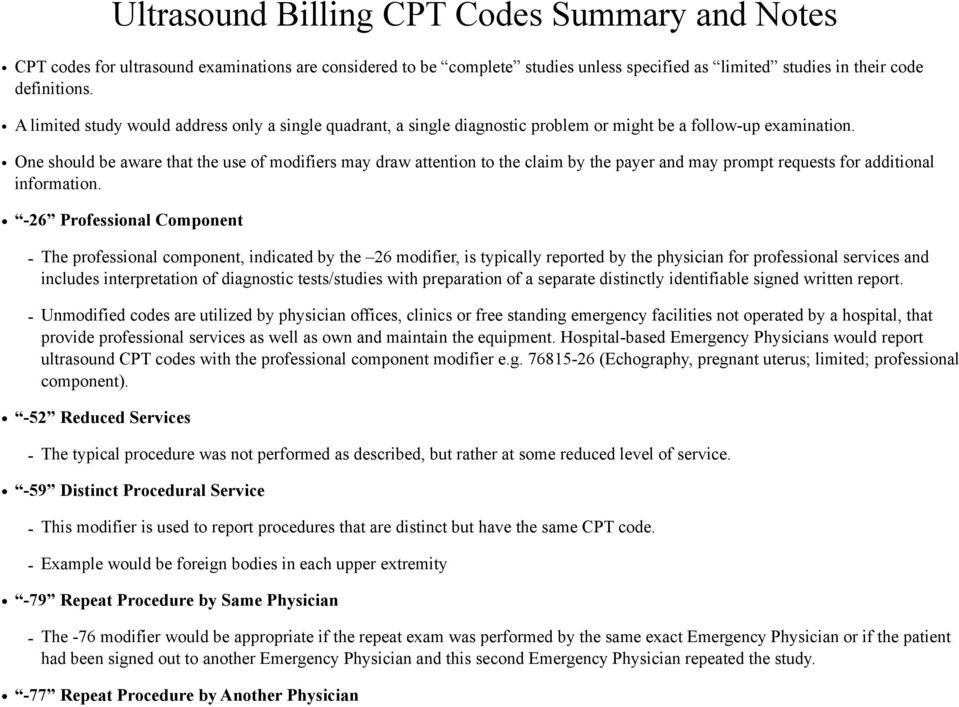
Aug 10, An ultrasound was performed solely for gestational dating which resulted in 9 weeks. I find the following diagnosis codes: Z, Z, Zxx. Apr 30, Obstetrical (OB) ultrasound studies must be well documented in order to support the CPT® code(s) chosen. The CPT code book lists the.
Results for perinatal death were as follows: Only 1 included trial assessed serious neonatal morbidity and found no evidence of group differences RR 0. For the comparison of a single Doppler assessment versus no Doppler, evidence for group differences in perinatal death was detected RR 0. However, these results are based on a single trial, and these researchers would recommend caution when interpreting this finding. There was no evidence of group differences for the outcomes of caesarean section, neonatal intensive care admissions or preterm birth of less than 37 weeks. Evidence for admission to neonatal intensive care unit was assessed as of moderate quality, and evidence for the outcomes of caesarean section and preterm birth of less than 37 weeks was graded as of high quality.
There was no available evidence to assess the effect on substantive long-term outcomes such as childhood neurodevelopment and no data to assess maternal outcomes, particularly maternal satisfaction. The authors concluded that existing evidence does not provide conclusive evidence that the use of routine umbilical artery Doppler ultrasound, or combination of umbilical and uterine artery Doppler ultrasound in low-risk or unselected populations benefits either mother or baby.
They stated that future studies should be designed to address small changes in perinatal outcome, and should focus on potentially preventable deaths. In a Cochrane review, Bricker et al evaluated the effects on obstetric practice and pregnancy outcome of routine late pregnancy ultrasound, defined as greater than 24 weeks' gestation, in women with either unselected or low-risk pregnancies.
These investigators searched the Cochrane Pregnancy and Childbirth Group's Trials Register May 31, and reference lists of retrieved studies. All acceptably controlled trials of routine ultrasound in late pregnancy defined as after 24 weeks were selected for analysis. Three review authors independently assessed trials for inclusion and risk of bias, extracted data and checked them for accuracy.
A total of 13 trials recruiting 34, women were included in the systematic review. Risk of bias was low for allocation concealment and selective reporting, unclear for random sequence generation and incomplete outcome data and high for blinding of both outcome assessment and participants and personnel. There was no difference in ante-natal, obstetric and neonatal outcome or morbidity in screened versus control groups.
Routine late pregnancy ultrasound was not associated with improvements in overall perinatal mortality.
There is little information on long-term substantive outcomes such as neurodevelopment. There is a lack of data on maternal psychological effects. Overall, the evidence for the primary outcomes of perinatal mortality, pre-term birth of less than 37 weeks, induction of labor and caesarean section were assessed to be of moderate or high quality with GRADE software. There was no association between ultrasound in late pregnancy and perinatal mortality RR 1.
Ultrasound for Pregnancy
Because none of the included studies reported these outcomes, they were not assessed for quality with GRADE software. The authors concluded that based on existing evidence, routine late pregnancy ultrasound in low-risk or unselected populations did not confer benefit on mother or baby. There was no difference in the primary outcomes of perinatal mortality, pre-term birth of less than 37 weeks, caesarean section rates, and induction of labor rates if ultrasound in late pregnancy was performed routinely versus not performed routinely.
Meanwhile, data were lacking for the other primary outcomes: The authors stated that these outcomes may warrant future research. The Zika virus is a mosquito-borne virus that has been associated with congenital defects, primarily of the central nervous system SMFM, According to the Centers for Disease Control and Prevention, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine, clinicians should screen pregnant women for possible Zika exposure, particularly if living or traveled to areas of active Zika transmission. Pregnant women exposed to Zika or who report clinical illness consistent with the virus should be tested for the virus based on national guidelines.
Part of that testing involves fetal ultrasound to detect microcephaly or intracranial calcifications, and in certain cases, amniocentesis may be offered SMFM, Bellussi and colleagues noted that fetal mal-positions and cephalic mal-presentations are well-recognized causes of failure to progress in labor. They frequently require operative delivery, and are associated with an increased probability of fetal and maternal complications. Traditional obstetrics emphasizes the role of digital examinations, but recent studies demonstrated that this approach is inaccurate and intra-partum US is far more precise.
These investigators summarized the available evidence and provided recommendations to identify mal-positions and cephalic mal-presentations with US. These researchers proposed a systematic approach consisting of a combination of trans-abdominal and trans-perineal scans and described the findings that allow an accurate diagnosis of normal and abnormal position, flexion, and synclitism of the fetal head.
The management of mal-positions and cephalic mal-presentation is currently a matter of debate, and individualized depending on the general clinical picture and expertise of the provider. The authors concluded that intra-partum US allows a precise diagnosis and thus offers the best opportunity to design prospective studies with the aim of establishing evidence-based treatment.
Castro and associates determined the diagnostic accuracy of US to detect deep-vein thrombosis DVT in pregnant patients. The reference lists of the included studies were analyzed. Original articles from accuracy studies that analyzed US to diagnose DVT in pregnant women were included. Reference standard was the follow-up time. Titles and summaries from 2, articles were identified; 4 studies that evaluated DVT in pregnant women were included; a total of participants were enrolled.
Negative predictive value was The authors concluded that accuracy of US to diagnose DVT in pregnant women was not determined due to the absence of data yielding positive results. They stated that further studies of low risk of bias are needed to determine the diagnostic accuracy of US in this clinical scenario. Not all components will be required. If any of the required fetal or maternal components are non-visualized due to fetal position, late gestational age, maternal habitus, etc. Follow-up ultrasound performed after a detailed anatomic ultrasound CPT code , should be reported as CPT Ultrasound, pregnant uterus, real time with image documentation, follow-up SMFM, Clinical Policy Bulletin Notes.
Links to various non-Aetna sites are provided for your convenience only. CPB - Fetal Echocardiograms.
CPT Codes by Specialty
As adjunct to chorionic villus sampling, embryo transfer, or localization and removal of an intra-uterine device To assess for certain fetal anomalies, such as anencephaly, in patients at high risk To confirm cardiac activity To confirm the presence of an intra-uterine pregnancy To diagnosis or evaluate multiple gestations To estimate gestational age To evaluate a suspected ectopic pregnancy To evaluate maternal pelvic or adnexal masses or uterine abnormalities To evaluate pelvic pain To evaluate suspected hydatidiform mole To evaluate vaginal bleeding To screen for fetal aneuploidy.
Standard Examination A standard ultrasound includes an evaluation of fetal presentation, amniotic fluid volume, cardiac activity, placental position, fetal biometry, and fetal number, plus an anatomic survey. A standard examination of fetal anatomy includes the following essential elements: Abdomen stomach, kidneys, bladder, umbilical cord insertion site into the fetal abdomen, umbilical cord vessel number.
Head, face and neck cerebellum, choroid plexus, cisterna magna, lateral cerebral ventricles, midline falx, cavum septi pellucidi, upper lip. Sex medically indicated in low-risk pregnancies only for the evaluation of multiple gestations. Who to scan, when to scan, and by whom. Obstet Gynecol Clin North Am. The routine obstetric ultrasound examination. Screening for chromosomal abnormality. Diagnostic ultrasound in pregnancy: The routine or screening obstetrical ultrasound examination. Gebauer C, Lowe N. Antepartal assessment of fetal well-being.
J Obstet Gynecol Neonatal Nursing. Routine ultrasound scanning in pregnancy. Ultrasound screening for fetal structural anomalies.
Curr Opin Obstet Gynecol. Obstetric ultrasound by family physicians. Ultrasound evaluation of the fetus. Guidelines for Perinatal Care. Elk Grove Village, IL: Guidelines for diagnostic imaging during pregnancy. Clinical Management Guidelines for Obstetrician-Gynecologists. Prenatal diagnosis of fetal chromosomal abnormalities. Guidelines and recommendations for safe use of Doppler ultrasound in perinatal applications.
J Matern Fetal Med. Ultrasonic assessment of the peri- and postmenopausal ovary. Ultrasonic assessment of the postmenopausal uterus. Three-dimensional ultrasound experience in obstetrics.
Three-dimensional ultrasound in gynecology: Amniocentesis and women with hepatitis B, hepatitis C, or human immunodeficiency virus. J Obstet Gynaecol Can. Ultrasound screening in pregnancy: A systematic review of the clinical effectiveness, cost-effectiveness and women's views. The use of first trimester ultrasound. Prenatal ultrasound as a screening test. ICSI; updated October Three-dimensional sonographic features of placental abnormalities. American College of Obstetricians and Gynecologists.